Today I will again tell you about lasers, cornea and vision correction. But this time we will not talk about the different versions of LASIK and ReLEx SMILE, but about the latest modifications of TransFRC. The method is all undeservedly kicked, calling obsolete and inferior in all other technologies. Plus, it is constantly confused with the usual PRK, despite the fact that between them really lies the technological abyss. I will try to show why this is not so, but at the same time I will tell why there are queues for us before we start recruiting to flight schools and educational institutions of the Ministry of Internal Affairs.
The cornea is a sandwich
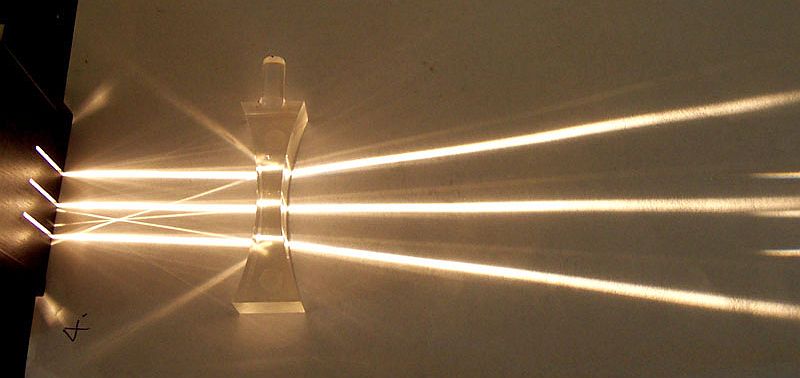
A refractive surgeon in designing an operation on the cornea is largely confronted with tasks similar to those that are solved by an optician who designs milling lenses on a CNC machine. Only the responsibility here is orders of magnitude higher - you will not take a new blank and you should ideally do it the first time. In order to get a lens from a conditional blank, you need to remove some of the original material. Only after that the lens begins to change the course of the rays as designed.
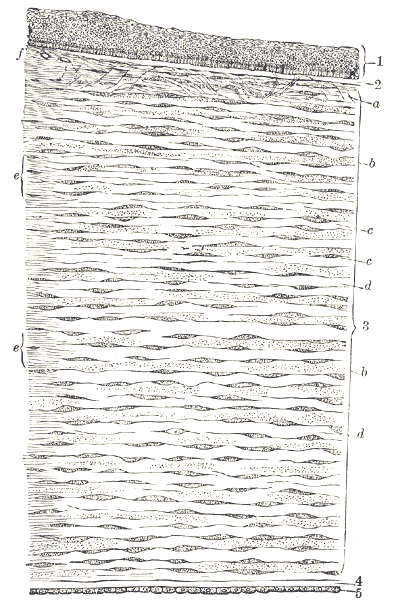
If we consider the original human cornea as a blank for a future lens, then we are especially interested in the stroma - the middle part of the tissue, which does not contain cells and consists of transparent fibers. It is in this layer that the laser will evaporate the planned volume in order to eventually correct the course of the rays. But the difficulty is that the top of the stroma is covered with epithelium, which acts as a protective layer. Therefore, to get to the middle can be different. The LASIK and Femto-LASIK methods assume that the doctor cuts the epithelium with a special blade or laser, evaporates the stroma area, and then puts the flap in place. ReLEx SMILE involves already more difficult cutting out the lens directly into the thickness of the cornea and removing it through a small incision. All of these methods have several problems.
Corneal thickness
The concept of refractive surgery from the point of view of physics is not fundamentally different from the creation of glasses. It is based on the same laws of optics. I think that everyone has seen thick lenses that very short-sighted people are forced to use with glasses. In order to make a big amendment to the original optical system, we have to take thick blanks in order to cut the lenses out of them with sufficient optical power. The same principle applies to surgery - the more conditional myopia we want to remove, the stronger and thicker the “lens” that will be created from the original cornea tissue. Roughly speaking, in order to correct myopia in -1.5D, very few tissues need to be removed. Points for correcting such a problem can also be very thin.
The lenses of glasses have one undoubted plus - we can almost always take a thicker blank. In extreme cases, we can replace the frame with a more massive one. But our own fabrics have a strictly limited limit, beyond which we have no right to go. It is of utmost importance for us that the corneal thickness remaining after correction meets strict safety standards. That is why there are cases when the doctor is forced to refuse the operation to a patient with a thin cornea. Or it offers a compromise with incomplete correction, since its tissues will be enough for only a correction from the conditional -12D to -4.5D. A special feature of TransFRC is that this technique preserves the architecture of the cornea better than many others. Moreover, this method is one of the most accurate. Due to its features, TransFRK allows to obtain the most individualized correction profile.
Nerve endings and dry eye syndrome
All methods of vision correction associated with changes in the geometry of the cornea, there are difficulties with nerve endings. The cornea is probably the most sensitive part of the body. It has 300-600 times more nerve endings than in the skin. Even supersensitive tooth pulp contains 20-40 times less sensory cells. When crossing a nerve, it almost always dies and very rarely is restored again. For the cornea, this loss of sensitivity often leads to difficulties with the blinking reflex, which is not activated in time. As a result, a certain percentage of people suffer from dry eye syndrome after correction. Despite the fact that everything does not sound so bad, chronic xerophthalmia can be a serious problem. There may be negative effects in terms of reduced visual acuity, and because of this, an inflammatory process can potentially occur. In the case of TransFRC, tissue evaporation proceeds as superficially as possible, affecting only those superficial nerve endings that lie at a depth of a few micrometers. With LASIK, the surface nerve endings are cut and deeper nerve endings are additionally damaged.
In normal PRK, the epithelium is removed mechanically. At the micro level, this is a fairly aggressive procedure, especially in terms of the formation of edges. In TransFRK, you literally do not need to touch any tools; everything is done by a precise laser. Contactless. The edge is as smooth as possible and the surface of the cornea is injured significantly less, which is important for subsequent regeneration. Actually, this is why Schwind calls this operation “touchless”.
Single Stage TransFRK
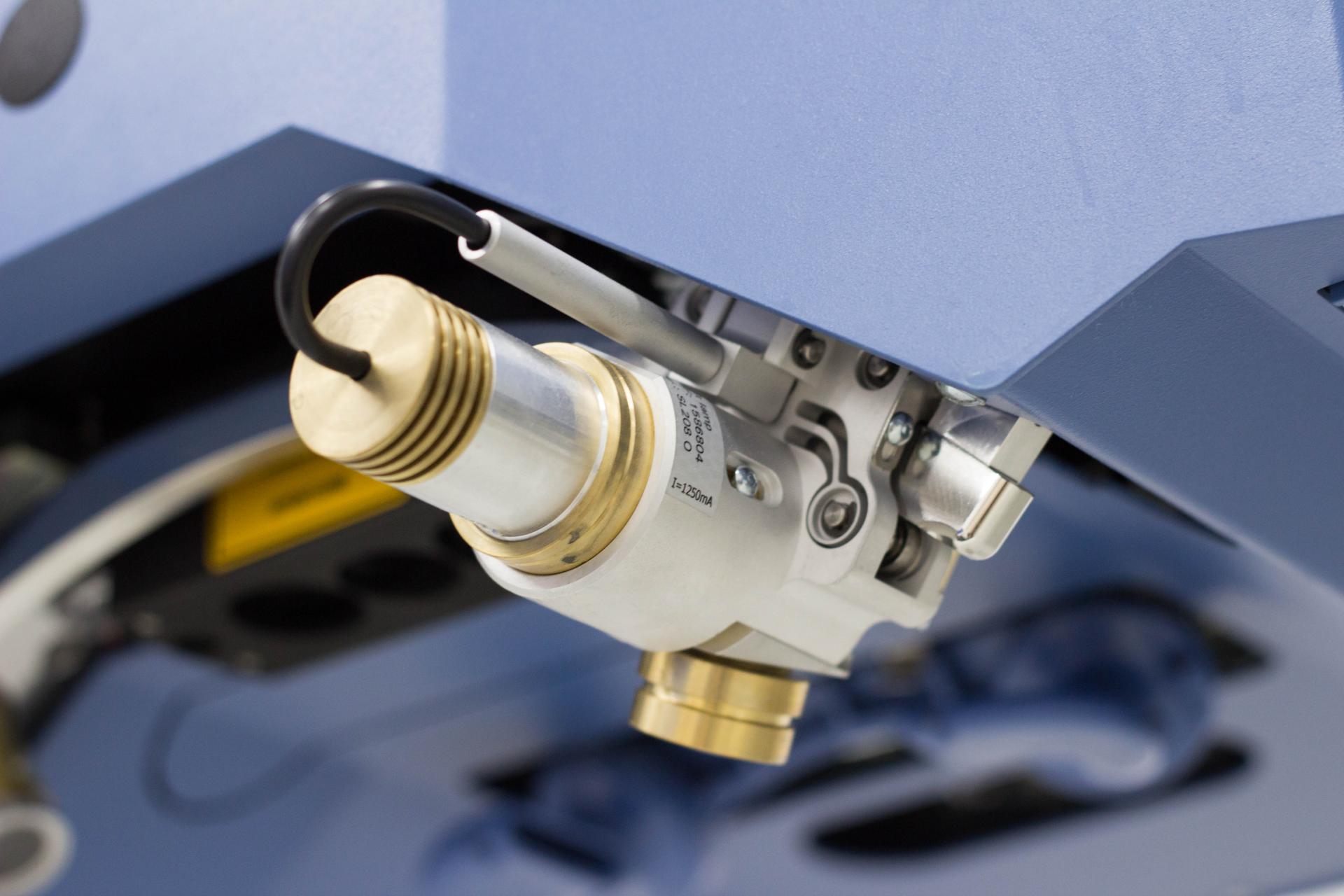
The Schwind AMARIS laser gives absolutely amazing results not only when performing Femto-LASIK, but also with TransFRC. He even repeatedly received prestigious awards, which are awarded for the best developments in the field of surgical equipment, in particular “Medical Design Excellence Award 2008” and “Industriepreis 2008”. The fact is that thanks to him, you can move from a two-stage version of the operation to a one-stage one. When TransFRC did not exist, the surgeon removed the corneal epithelium mechanically, with a special scraper, or after treatment with alcohol. With the advent of TransFRC in 1998, it was possible to abandon the mechanical impact. But there was one more problem. Two stage. At the first stage, the surgeon evaporated the epithelium with the laser using the PTK method - uniform ablation of the refractive component that does not contain (it is still used now in some cases), and he had to work with a laser solely by subjective criteria. When the laser finished with the evaporation of the epithelium and began to remove the stroma, the fluorescence of the treated surface changed and the surgeon had to catch this moment in time. After that, downloading a new program to the laser computer, he began the second, refractive stage. All this contributed undesirable errors in the result. For example, the epithelium of the central zone of the cornea was the first to be removed - it is thinner and the periphery of the cornea is curved and less laser energy reaches it. Thus, it was removed or more than the need tissue or the optical zone of the operation was greatly reduced reducing the quality of vision. When switching between programs, the cornea dried out and the accuracy of the operation decreased.
The one-step technology completely eliminated the human factor, took into account energy losses in the periphery, the need to control the temperature of the cornea, and in fact the main task of the surgeon was to design the future profile of the cornea. Then the machine performs everything itself, excluding the human factor. The resolution of ablation is
250 nm ! You can even conditional staphylococcus cut into neat slices.
Technology features
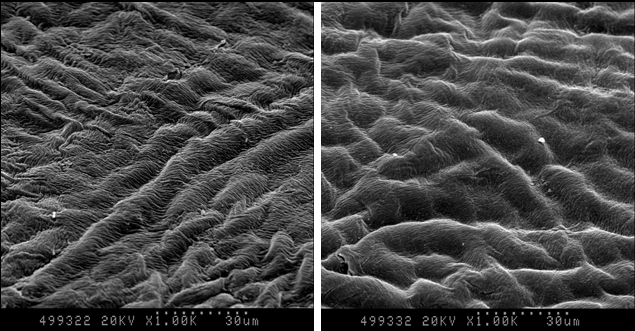 Image courtesy of Dr. David Kang, Eyereum, Korea.
Image courtesy of Dr. David Kang, Eyereum, Korea.The SmartPulse technology was launched by Schwind into clinical practice in 2015. She allowed to create a much smoother profile of the surface of the cornea after treatment. They created a new mathematical model that made it possible to more accurately perform the evaporation of tissues with a laser. This quality of the final surface has many advantages. First, more accurate results are achieved from the point of view of refraction - in humans, the final vision is better than when using old technology. Secondly, the smooth surface is very fond of epithelial cells. They restore the cornea, “creeping” from the periphery to the center and do not like very much when the profile has irregularities. In such cases, there may even be complications in the form of cloudiness - Haze. After AMARIS with its SmartPulse it is practically excluded.
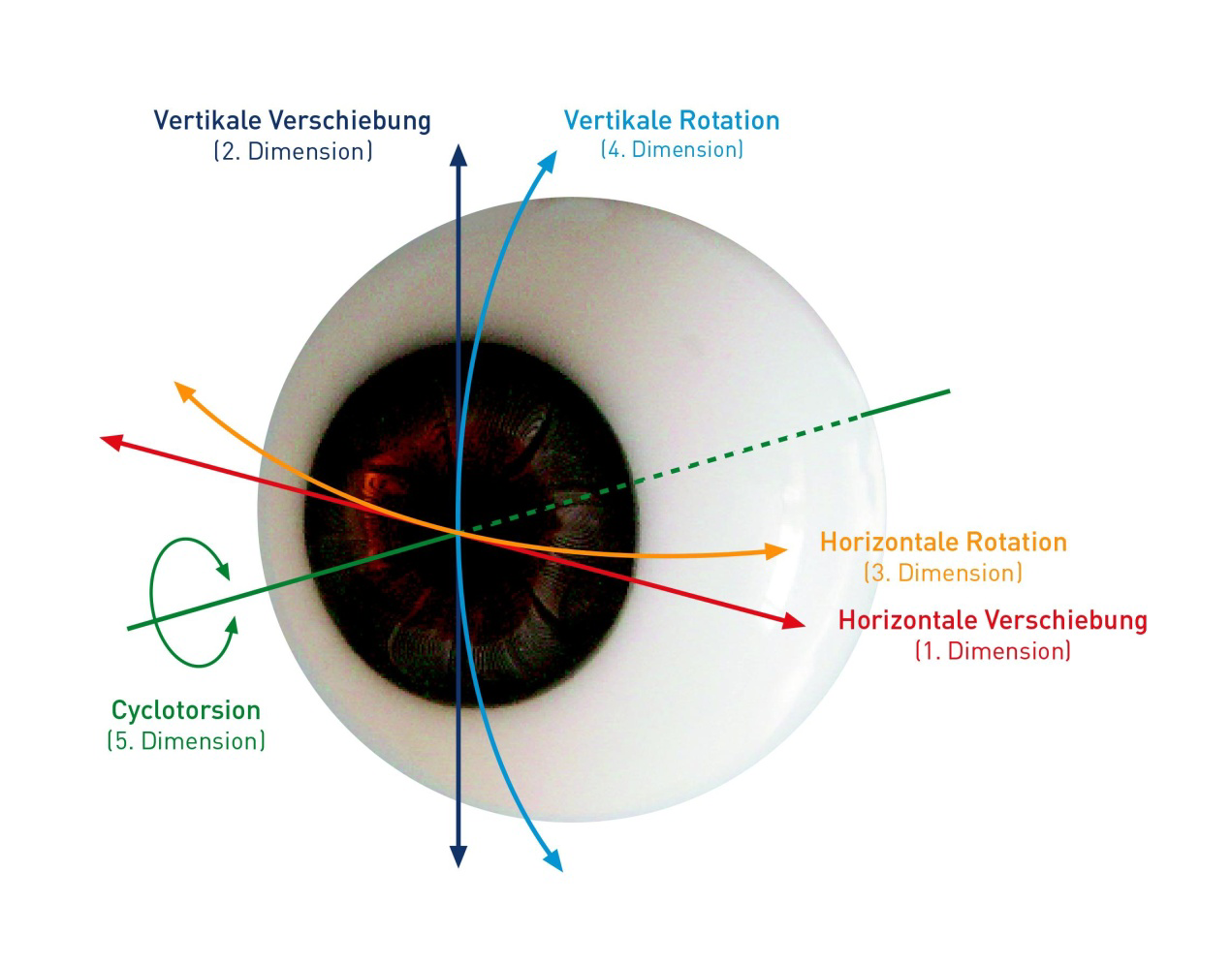
Eye micromovements are compensated by the automatic tracking system. We cannot be perfectly still and our eyes move even in response to the heartbeat. At the expense of tracking Amaris controls the movement of the eyes in five degrees of freedom. Even if you pull, the laser will, until the last moment, fall exactly where it was planned, and then just turn off and swear at you until the eye returns to the allowed area again.
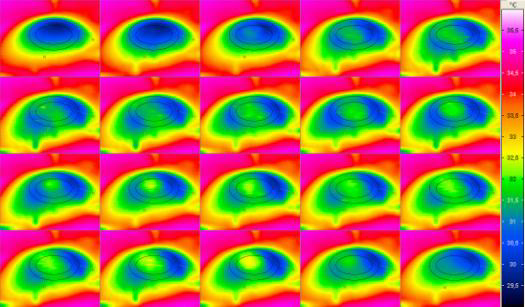
Thermal control is carried out by the camera, fixing the far infrared range. In this case, the laser shoots all the time in different parts of the cornea to prevent it from overheating. As a result, with sufficiently rapid evaporation of the desired volume of tissue, we precisely control the temperature.
SCHWIND CAM in a Schwind AMARIS 500E installation, scans the surface of the cornea pointwise, performs the maximum number of individual measurements of the cornea, not only general indicators, takes into account the difference in the ablation coefficient between the epithelium and the cornea and the energy loss of the beam caused by the change in corneal curvature from the center to the periphery (radius of curvature of the cornea). That is, the laser not only works as an installation with CNC, but also as an ultra-precise realtime 3D scanner, which gives feedback.
No trace
One of the interesting features of TransFRK is the complete absence of traces of exposure after a few months. In a sense in general. If you do not perform an accurate cornea scan with a measurement of its thickness over the entire volume, then no slit-lamp examinations will even give reason to suspect that a correction has been made. TransFRC at the moment is a method with minimal impact on the architecture of the cornea and with a very low percentage of complications. Actually, it is just before each set of flight schools that many patients adjust their vision for themselves to successfully complete the commission. No problems with overload, extreme conditions in these patients does not arise due to the minimal impact. In most countries, this is the only technology that allows you to subsequently serve in the armed forces and rescue services.
We have accumulated a large amount of statistical data on our patients. I think that we will slightly reveal the full statistics on various technologies in subsequent posts, still sensitive data. But now we can say that TransFRK gives very good long-term results (after 6 months): 98% of patients have a deviation of no more than 0.5 diopters from the planned refraction. These small fluctuations fit into the individual characteristics of the regeneration of corneal tissue and are almost imperceptible. Compared with conventional PRK, pain syndrome is much less pronounced, but in most patients it practically disappears within a few days, taking into account the prescription of anti-inflammatory drugs. Some have none at all, even without pills. We even had a patient who asked for permission to get behind the wheel on the day of the operation, since nothing bothered him. His refraction was excellent, so we resolved. True, he will have to change his rights in order to remove the mark about the need to wear glasses or contact lenses while driving.
Traditional bonuses
As a result of our first post with the quest, we played a lot of different prizes and, with a free correction certificate, we just completed TransFRC - for the Victoria patient, this turned out to be the best option possible. There are no new certificates yet, but we decided to issue a discount for correction using this technology
until August 31, inclusive . The usual price, depending on the complexity, varies within 34,000 - 47,000 per eye, but according to the Geektimes code you will receive 5,000 discounts for each eye.
Contacts:"Ophthalmological clinic" Sphere "by Professor Eskina"
call center telephone: +7 (495) 480-75-84
our address: Moscow, st. Starokachalovskaya, 6